The AI-STROKE project uses AI to employ dry EEG for quickly identify severity of strokes before hospital arrival, speeding up treatment in countries such as the Netherlands where the hospital assigned to the patient is dependent on the severity level. In this video, the ANT Neuro team is in conversation with the main researchers and the paramedics to understand the practical and infrastructural concerns in their effort to push ahead the ideology that “Time is Brain”.
Meet the researchers
The AI-STROKE project brings together a multi-disciplinary research team from the Neurology, Biomedical Engineering and Physics; as well as the Radiology and Nuclear Medicine Departments of Amsterdam UMC (University Medical Centers). The project idea came about after the team recognized the need for a prehospital stroke triage method that routes each stroke patient directly to the right treatment. The project is being led by Jonathan Coutinho, MD PhD, who is a stroke neurologist at Amsterdam UMC and Wouter Potters, PhD, technical physician at Amsterdam UMC. They are joined in this endeavor by Henk Marquering, PhD, who is also Professor of Translational Artificial Intelligence in Amsterdam UMC. At the core of the project are the two PhD candidates, Maritta van Stigt, MSc and Eva Groenendijk, MSc. Both Maritta and Eva are technical physicians at Amsterdam UMC and drive the project forward in cooperation with ambulance stations and personnel across the Netherlands.
The AI-STROKE project also built the foundation of the newly established company TrianecT, which
intends to valorise the project technology and bring it to the market. Wouter leads TrianecT with
Jonathan and Henk as co-founders. Dr. Frank Zanow (CEO, Neuromotion Ventures) also joins
them as a co-founder in TrianecT. The mission statement of TrianecT is to get stroke patients to the
right hospital for the right treatment without delays.

Figure 1: Team AI-STROKE (from left to right): Wouter Potters, Jonathan Coutinho, Maritta van Stigt, Eva Groenendijk, Henk Marquering.
Project motivation and objectives
Acute ischemic stroke (AIS) affects 9 million people per year worldwide, and large vessel occlusion (LVO) stroke patients make up about a quarter to a third of that number [1]. LVO stroke patients are potentially eligible for endovascular thrombectomy (EVT), which is a procedure that needs to be initiated urgently to increase the chance of good patient outcomes [2].
Intravenous thrombolysis (IVT) has been the standard treatment for acute ischemic stroke, and in 2015, a combination of trials established the efficacy of EVT for patients with large vessel occlusion stroke of the anterior circulation (LVO-a) [3]. EVT has since then been adopted as the standard therapy for this patient group.
EVT can only be performed in comprehensive stroke centers (CSCs); however, all suspected stroke patients are transported to the nearest hospital, often a primary stroke center (PSC) (Figure 2). Once a CT scan confirms that the patient has an LVO-a stroke, they are transported again to the CSC for endovascular treatment. This leads to a 1-hour delay which worsens the outcome of those patients.
The AI-STROKE project and researchers therefore propose to triage suspected stroke patients in a prehospital setting, so they can be directly brought to a CSC without losing any time [4,6,7].
In the AI-STROKE project, the team uses electroencephalography (EEG) and artificial intelligence algorithms to reliably predict LVO-a stroke. Dry EEG fulfills all the criteria for a successful prehospital triage tool: high diagnostic accuracy; fast application and interpretation; user-friendliness; compactness; and low costs [4].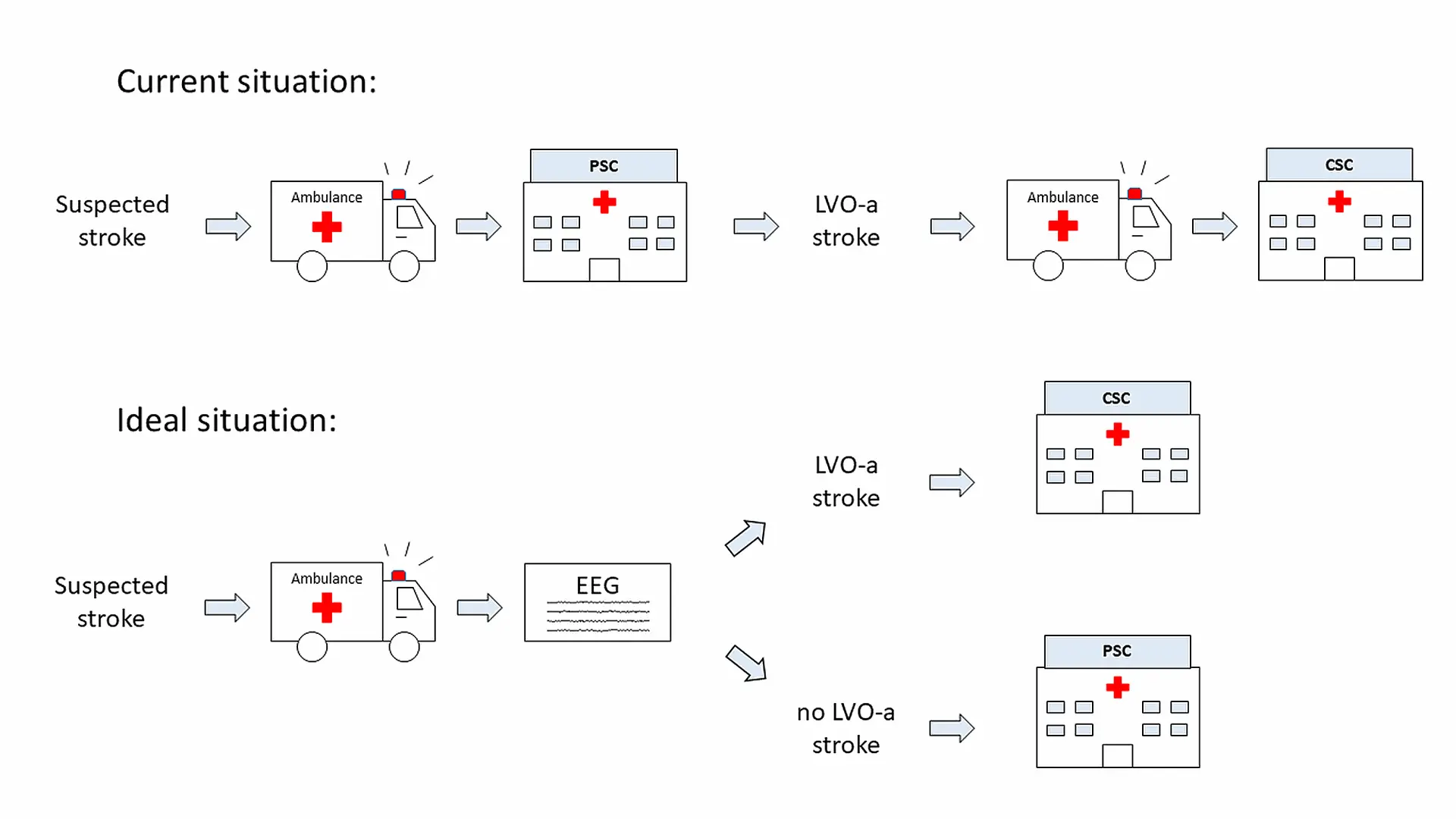
Figure 2: The differences between the current and proposed ideal prehospital workflow
for suspected stroke patients [6].
AI-Stroke – Study overview
In the initial phase of the project, ambulance stations across the Netherlands (Ambulance Amsterdam and Witte Kruis Ambulancezorg Alkmaar) are collaborating with the team at Amsterdam UMC to collect EEG data from suspected stroke patients. Patients who are referred to a participating hospital (Amsterdam UMC, OLVG Hospital, and Noordwest Ziekenhuisgroep) are included. Patients clinically suspected of having a stroke as judged by the ambulance personnel, are 18 years of age or older, and their symptoms started <24 hours before the start time of the EEG recording are included. The main exclusion criteria for this study are skin lesions or infections on the head or a (suspected) COVID-19 infection. Based on the above criteria, dry EEG data are recorded from the suspected stroke patients by the ambulance personnel in the prehospital setting. This group are trained in advance by the research team and are even provided small info sheets (Figure 3). The hardware is packed into an easy to carry, transportable suitcase that is placed in a dedicated station inside the ambulance. The dry EEG recordings are carried out either at the patient’s site or inside the ambulance before transport to the nearest PSC. During measurements patients lie supine. Such prerequisites reduce movement and muscle contraction to ensure that the recorded data is as clean as possible.
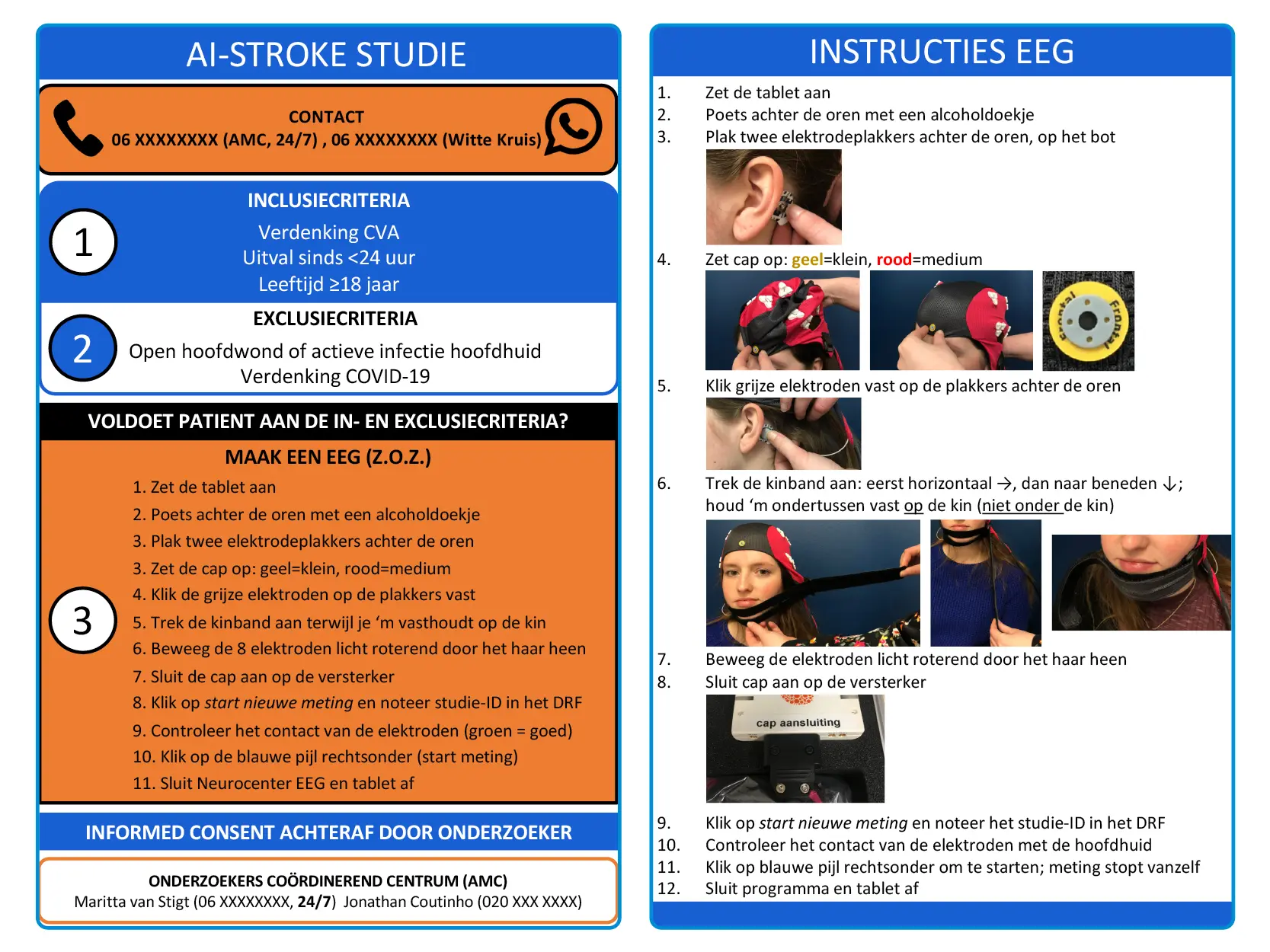
Figure 3: The infosheet provided to participating ambulance stations. The instructions are written in Dutch.
To ensure that minimal time is spent in this prehospital setting, the recording software has time limits imposed on every step in the acquisition software. The electrode positioning step where the ambulance personnel optimize electrode-skin contact, is limited to a maximum of 1.5 minutes. The EEG recording then lasts for a maximum of 3 minutes. The acquired data are end-to-end encrypted sent to Amsterdam UMC so that these can be analyzed in retrospect.
After obtaining informed consent, for each patient, a copy of the clinical hospital records (demographics, medical history, and medication) is obtained along with the EEG data and stored securely such that only the researchers can access it for their analysis [3].
Technology incorporated in the study
The acute care setting and aim of this study demand the use of fast cap application measures, easy-to-use equipment, good data quality and intuitive acquisition software. The AI-STROKE study makes use of a specially developed 8 channel waveguardTMtouch cap with electrodes positioned at 10/20 locations FC3, FC4, CP3, CP4, FT7, FT8, TP7, TP8. The reference and the ground electrodes are designed to be external drop-leads with flat snap electrodes which can be attached to hydrogel sticker electrodes and placed behind either ear on the mastoids.
At each of the electrode locations, a dry
electrode triplet has been placed to act as
one individual electrode. This increases the
surface area of scalp contact at each location.
Externally, this arrangement also increases
the stability of the electrode at each location
and prevents any tilting of the electrode,
thereby optimizing electrode-skin contact.
This cap also includes an adapted chinstrap
with Velcro so that strapping and cap
application can be relatively faster. Most of
all, this waveguardTM touch cap ensures the
ease of use of the equipment by ambulance
personnel that are not traditionally trained
on EEG measurement methods. The cap
is connected to an 8 channel eegoTM mini
amplifier which is permanently connected to
the tablet with the EEG recording software to
reduce time in hardware preparations.
The NeuroCenter® EEG software (Clinical
Science Systems, Leiden, The Netherlands)
is used to record the dry EEG data. The
equipment is connected to a tablet that runs
this acquisition software within which the
eegoTM SDK is deployed.
Planned analysis
The EEG analysis plan includes a first artifact detection and detection step. Then, EEG features among which the relative delta, theta, alpha and beta power estimation, delta/alpha and theta/alpha ratios as well as delta+theta/alpha+beta ratio are calculated. With these features, a logistic regression algorithm for the detection of LVO-a stroke will be developed. Once more data becomes available, neural networks will be trained with either EEG features or raw EEG data as input. The Nicolab team (Amsterdam, the Netherlands) contributes to this phase by providing their expertise on Artificial Intelligence (AI) to the AI-STROKE project.
Future outlook
This project is not only ground-breaking for
prehospital stroke triage, but it also sheds
light on the technological challenges in acute
stroke research. Primarily, this project shows
the need for time-efficient neuroimaging
measurement methods such as dry EEG
and the feasibility of using dry EEG in an
emergency environment. This project has
received significant interest and publicity
even in national organizations such as the
Tweede Kamer (House of Representatives,
The Netherlands). ANT Neuro is proud to
collaborate with the AI-STROKE team and
the TrianecT team, we hope this research will
transform the prehospital stroke care chain in
the near future.
References
Malhotra, Konark, Jeffrey Gornbein, and Jeffrey L. Saver. “Ischemic strokes due to large-vessel occlusions contribute disproportionately to stroke-related dependence and death: a review.” Frontiers in neurology 8 (2017): 651.
Saver, Jeffrey L., et al. “Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis.” Jama 316.12 (2016): 1279-1289.
Goyal, Mayank, et al. “Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials.” The Lancet 387.10029 (2016): 1723-1731.
van Meenen, Laura CC, et al. “Detection of large vessel occlusion stroke in the prehospital setting: Electroencephalography as a potential triage instrument.” Stroke 52.7 (2021): e347-e355.
Murray, Nick M., et al. “Artificial intelligence to diagnose ischemic stroke and identify large vessel occlusions: a systematic review.” Journal of neurointerventional surgery 12.2 (2020): 156-164.
van Stigt, Maritta N., et al. “ELECTRA-STROKE: Electroencephalography controlled triage in the ambulance for acute ischemic stroke—Study protocol for a diagnostic trial.” Frontiers in Neurology 13 (2022).
van Meenen, Laura CC, et al. “Detection of large vessel occlusion stroke with electroencephalography in the emergency room: first results of the ELECTRA-STROKE study.” Journal of neurology 269.4 (2022): 2030-2038.